Total Knee Replacement Guide
DR. SAKSHAM MITTAL
JOINT REPLACEMENT SPECIALIST
If your knee is severely damaged by arthritis it may be hard for you to perform simple activities, such as walking or climbing stairs. You may even begin to feel pain while you are sitting or lying down.
If nonsurgical treatments like medications and using walking supports are no longer helpful, you may want to consider total knee replacement/resurfacing surgery. Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities.
Total knee replacements are one of the most successful procedures in all of medicine. Improvements in surgical materials and techniques have greatly increased its effectiveness.
Whether you have just begun exploring treatment options or have already decided to have total knee replacement surgery, this article will help you understand more about this valuable procedure.
Anatomy
The knee is the largest joint in the body and having healthy knees is required to perform most everyday activities.

The knee is made up of the lower end of the thighbone (femur), the upper end of the shinbone (tibia), and the kneecap (patella). The ends of these three bones are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily within the joint.
The menisci are located between the femur and tibia. These C-shaped wedges act as shock absorbers that cushion the joint.
Large ligaments hold the femur and tibia together and provide stability. The long thigh muscles give the knee strength.
All remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage, reducing friction to nearly zero in a healthy knee.
Normally, all of these components work in harmony. But disease or injury can disrupt this harmony, resulting in pain, muscle weakness, and reduced function.
Causes
The most common cause of chronic knee pain and disability is arthritis. Although there are many types of arthritis, most knee pain is caused by just three types: osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
Osteoarthritis:
This is an age-related wear and tear type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the knee softens and wears away. The bones then rub against one another, causing knee pain and stiffness.
Osteoarthritis often results in bone rubbing on bone. Bone spurs are a common feature of this form of arthritis.

Rheumatoid arthritis:
This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed “inflammatory arthritis.”
Post traumatic arthritis:
This can follow a serious knee injury. Fractures of the bones surrounding the knee or tears of the knee ligaments may damage the articular cartilage over time, causing knee pain and limiting knee function.
What is done in surgery?
A knee replacement (also called knee arthroplasty) might be more accurately termed a knee “resurfacing” because only the surface of the bones are replaced.
There are four basic steps to a knee replacement procedure:
- Prepare the bone.The damaged cartilage surfaces at the ends of the femur and tibia are removed along with a small amount of underlying bone.
- Position the metal implants.The removed cartilage and bone are replaced with metal components that recreate the surface of the joint. These metal parts may be cemented or “press-fit” into the bone.
- Resurface the patella.The undersurface of the patella (kneecap) is cut and resurfaced with a plastic button. Some surgeons do not resurface the patella, depending upon the case.
- Insert a spacer.A medical-grade plastic spacer is inserted between the metal components to create a smooth gliding surface.

(Left) Severe osteoarthritis. (Right) The arthritic cartilage and underlying bone has been removed and resurfaced with metal implants on the femur and tibia. A plastic spacer has been placed in between the implants.
Is Total Knee Replacement for You?
The decision to have total knee replacement surgery should be a cooperative one between you, your family and your orthopaedic surgeon.
When Is Surgery Recommended?
There are several reasons why your doctor may recommend knee replacement surgery. People who benefit from total knee replacement often have:
- Severe knee pain or stiffness that limits everyday activities, including walking, climbing stairs, and getting in and out of chairs. It may be hard to walk more than a few blocks without significant pain and it may be necessary to use a cane or walker
- Moderate or severe knee pain while resting, either day or night.
- Chronic knee inflammation and swelling that does not improve with rest or medications.
- Knee deformity — a bowing in or out of the knee
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, lubricating injections, physical therapy, or other surgeries
Candidates for Surgery
There are no absolute age or weight restrictions for total knee replacement surgery.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total knee replacement are aged 50 to 80, but orthopaedic surgeons evaluate patients individually. Total knee replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether total knee replacement is the best method to relieve your pain and improve your function.
Other treatment options — including medications, injections, physical therapy, or other types of surgery — will also be considered and discussed.
In addition, your orthopaedic surgeon will explain the potential risks and complications of total knee replacement, including those related to the surgery itself and those that can occur over time after your surgery.
HOW YOUR XRAY LOOKS LIKE IN ARTHRITIS?
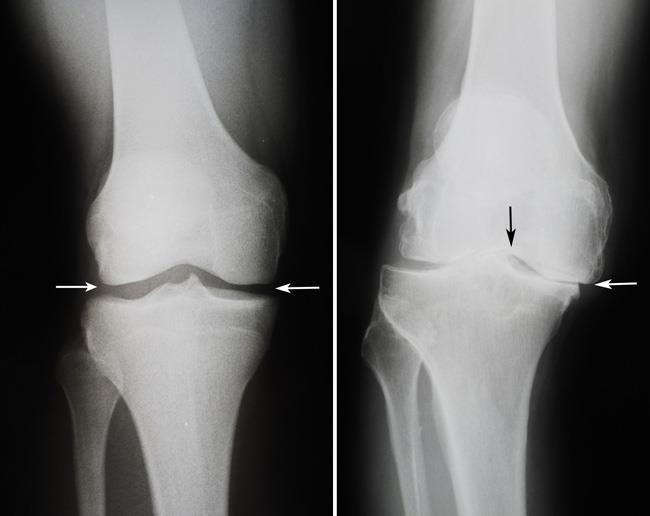
X RAY SHOWING DECREASED JOINT SPACE SUGGESTIVE OF ARTHRITIS
Confused/ Afraid to Have Knee Replacement Surgery?
Realistic Expectations
An important factor in deciding whether to have total knee replacement surgery is understanding what the procedure can and cannot do.
Most people who have total knee replacement surgery experience a dramatic reduction of knee pain and a significant improvement in the ability to perform common activities of daily living. But total knee replacement will not allow you to do more than you could before you developed arthritis.
With normal use and activity, every knee replacement implant begins to wear in its plastic spacer. Excessive activity or weight may speed up this normal wear and may cause the knee replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports for the rest of your life after surgery.
Realistic activities following total knee replacement include unlimited walking, swimming, golf, driving, light hiking, biking, ballroom dancing, and other low-impact sports.
With appropriate activity modification, knee replacements can last for many years (15-20 years).
Possible Complications of Surgery
The complication rate following total knee replacement is low. Serious complications, such as a knee joint infection, occur in fewer than 2% of patients. Major medical complications such as heart attack or stroke occur even less frequently. Chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur, they can prolong or limit full recovery.
Discuss your concerns thoroughly with your orthopaedic surgeon prior to surgery.
Infection. Infection may occur in the wound or deep around the prosthesis. It may happen within days or weeks of your surgery. It may even occur years later. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis. Any infection in your body can spread to your joint replacement.
Blood clots. Blood clots in the leg veins are one of the most common complications of knee replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Your orthopaedic surgeon will outline a prevention program, which may include periodic elevation of your legs, lower leg exercises to increase circulation, support stockings, and medication to thin your blood.
Implant problems. Although implant designs and materials, as well as surgical techniques, continue to advance, implant surfaces may wear down and the components may loosen. Additionally, although an average of 115° of motion is generally anticipated after surgery, scarring of the knee can occasionally occur, and motion may be more limited, particularly in patients with limited motion before surgery.
Continued pain. A small number of patients continue to have pain after a knee replacement. This complication is rare, however, and most patients experience excellent pain relief following knee replacement.
Neurovascular injury. While rare, injury to the nerves or blood vessels around the knee can occur during surgery.
Though these are the reported complications and are rare but as a patient it should be your right to be informed about them. Overall the surgery has a 99.9 percent success rate.
Preparing for Surgery
Tests
Several tests, such as blood and urine samples, and an electrocardiogram, echo etc. , may be needed to help your orthopaedic surgeon plan your surgery.
Medications
Tell your orthopaedic surgeon about the medications you are taking. He or she will tell you which medications you should stop taking (some blood thinners need to be stopped a week before surgery) and which you should continue to take before surgery.
Social Planning
Although you will be able to walk with a cane, crutches, or a walker soon after surgery, you will need help for several weeks with such tasks as cooking, shopping, bathing, and doing laundry.
If you live alone, a social worker or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at home. They also can help you arrange for a short stay in an extended care facility during your recovery if this option works best for you.
Home Planning
Several modifications can make your home easier to navigate during your recovery. The following items may help with daily activities:
- Secure handrails along your stairways
- A stable chair for your early recovery with a firm seat cushion (and a height of 18 to 20 inches), a firm back, two arms, and a footstool for intermittent leg elevation
- A toilet seat riser with arms, if you have a low toilet
A stable shower bench or chair for bathing
Your HOSPITAL JOURNEY (5-6 DAYS IN HOSPITAL)
You will either be admitted to the hospital on the day or a day before of your surgery,
Anesthesia
Upon arrival at the hospital, you will be evaluated by a member of the anesthesia team. The most common type of anesthesia is spinal with epidural / regional nerve blocks (you are awake but your body is numb from the waist down). The epidural catheter will remain in your back for pain control for the next 2-3 days which will be removed then.
Procedure
The surgical procedure usually takes 1 hour per knee. Your orthopaedic surgeon will remove the damaged cartilage and bone, and then position the new metal and plastic implants to restore the alignment and function of your knee.
Different types of knee implants are used to meet each patient’s individual needs. The surgeon is the best judge regarding the type and design of implant to be used and patient should trust the surgeon’s expertise on that,
Pain Management
Patients are most commonly afraid due to pain after surgery. After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster. Various pain reduction techniques are used to help the patient.
Blood Clot Prevention
Your orthopaedic surgeon may prescribe one or more measures to prevent blood clots and decrease leg swelling. These may include DVT pumps, compression stockings and blood thinners.Foot and ankle movement is also encouraged immediately following surgery to increase blood flow in your leg muscles to help prevent leg swelling and blood clots.
Physical Therapy
Most patients can begin walking and exercising their knee hours after surgery. A physical therapist will teach you specific exercises to strengthen your leg and restore knee movement to allow walking and other normal daily activities soon after your surgery. Physiotherapy is a very important part to achieve good results and should not be neglected. You may need to continue physiotherapy for 3- 4 weeks after surgery.
Your Recovery at Home
The success of your surgery will depend largely on how well you follow your orthopaedic surgeon’s instructions at home during the first few weeks after surgery.
Wound Care
You will have stitches or staples running along your wound or a suture beneath your skin on the front of your knee. The stitches or staples will be removed mostly after 2 weeks. A suture beneath your skin will not require removal. Avoid soaking the wound in water until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with a dietary supplement, is important to help your wound heal and to restore muscle strength.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal activities of daily living within 3 to 6 weeks following surgery. Some pain with activity and at night is common for several weeks after surgery.
Your activity program should include:
- A graduated walking program — initially in your home and later outside — to slowly increase your mobility
- Resuming other normal household activities, such as sitting, standing, and climbing stairs
- Specific exercises several times a day to restore movement and strengthen your knee. You probably will be able to perform the exercises without help, but you may have a physical therapist help you at home or in a therapy center the first 2-3 weeks after surgery.
You will most likely be able to resume driving when your knee bends enough that you can enter and sit comfortably in your car, and when your muscle control provides adequate reaction time for braking and acceleration. Most people resume driving approximately 4 to 6 weeks after surgery.
Avoiding Problems After Surgery
Warning signs :-
- Increasing pain in your calf
- Tenderness or redness above or below your knee
- New or increasing swelling in your calf, ankle, and foot
- Warning signs of pulmonary embolism.The warning signs that a blood clot has traveled to your lung include:
- Sudden shortness of breath
- Sudden onset of chest pain
- Localized chest pain with coughing
Preventing Infection
A common cause of infection following total knee replacement surgery is from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your knee replacement and cause an infection.
After knee replacement, patients with certain risk factors may need to take antibiotics prior to dental work, including dental cleanings, or before any surgical procedure that could allow bacteria to enter the bloodstream. Your orthopaedic surgeon will discuss with you whether you need to take preventive antibiotics before dental procedures.
Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible knee replacement infection:
- Persistent fever (higher than 100°F orally)
- Chills
- Increasing redness, tenderness, or swelling of the knee wound
- Drainage from the knee wound
- Increasing knee pain with both activity and rest
How Your New Knee Is Different
Improvement of knee motion is a goal of total knee replacement, but restoration of full motion is uncommon. The motion of your knee replacement after surgery can be predicted by the range of motion you have in your knee before surgery. Most patients can expect to be able to almost fully straighten the replaced knee and to bend the knee sufficiently to climb stairs and get in and out of a car. Kneeling is sometimes uncomfortable, but it is not harmful.
Most people feel some numbness in the skin around their incisions. You also may feel some stiffness, particularly with excessive bending activities.
Most people also feel or hear some clicking of the metal and plastic with knee bending or walking. This is normal. These differences often diminish with time and most patients find them to be tolerable when compared with the pain and limited function they experienced prior to surgery.
Your new knee may activate metal detectors required for security in airports and some buildings. Tell the security agent about your knee replacement if the alarm is activated.
Protecting Your Knee Replacement
After surgery, make sure you also do the following:
- Participate in regular light exercise programs to maintain proper strength and mobility of your new knee.
- Take special precautions to avoid falls and injuries. If you break a bone in your leg, you may require more surgery.
- See your orthopaedic surgeon periodically for routine follow-up examinations and X-rays. Your surgeon will talk with you about the frequency and timing of these visits.
DR. SAKSHAM MITTAL
JOINT REPLACEMENT AND SPORTS INJURY SPECIALIST
COMPUTER NAVIGATION/ ROBOTIC KNEE REPLACEMENT TRAINED SURGEON
CONSULTANT ORTHOPEDICS
CK BIRLA HOSPITAL, PUNJABI BAGH
MAHARAJA AGRASEN HOSPITAL, DWARKA
CONTACT: 7035823472
Visit our website for patient testimonials and surgery videos
www.drsakshamjointspecialist.com
OUR CLINIC: DR. MITTAL’S ORTHOPEDIC AND PHYSIOTHERAPY CENTER
A-3/122 PASCHIM VIHAR
9.30M A.M. – 12.30 P.M. DAILY (EXCEPT THURSDAY AND SUNDAY)
